Myelomeningocele’s two most common conditions associated with the brain are Hydrocephalus and Arnold Chiari II Malformation (pronounced key – ar- ee). In this article, we will discuss Hydrocephalus and the need for shunts in a person with Spina Bifida.
What is Hydrocephalus?
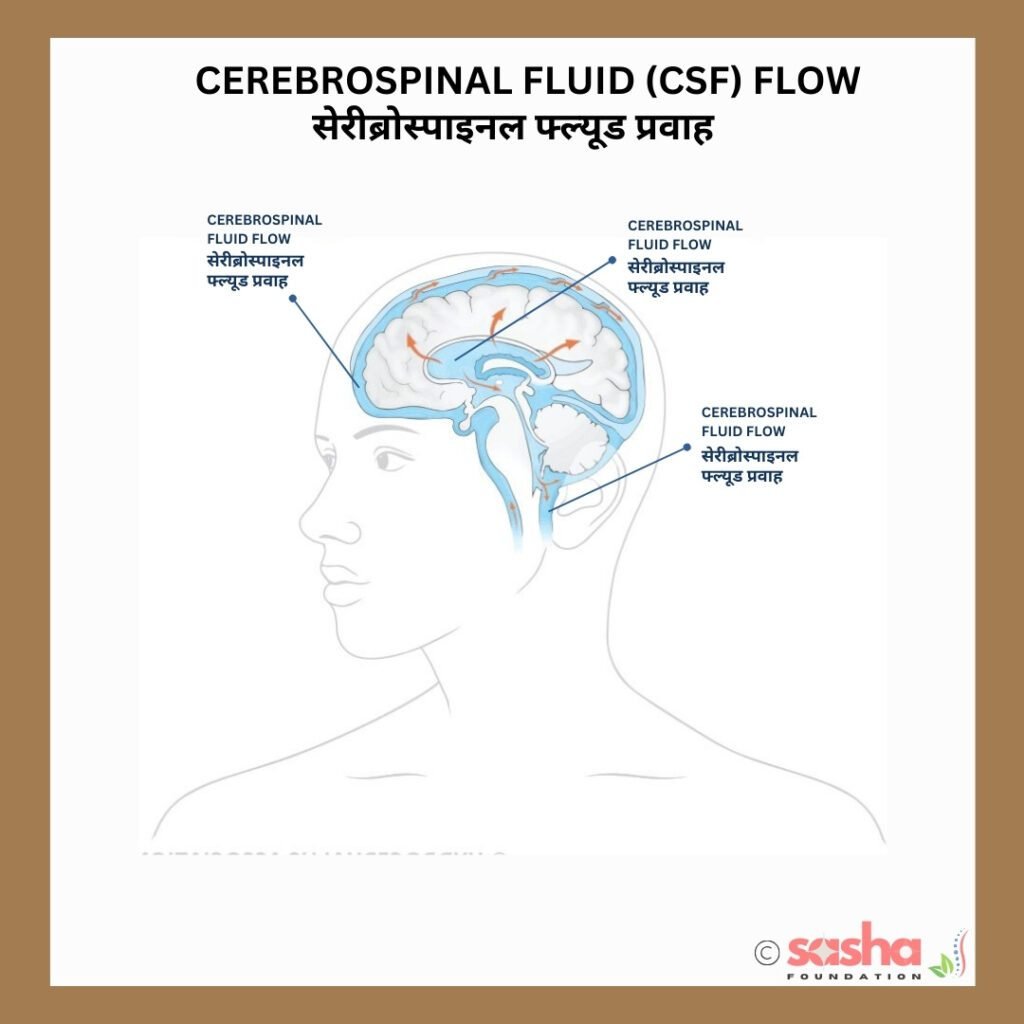
The brain continuously produces and is surrounded by a clear, salt-water-like special fluid, called cerebrospinal fluid (CSF) (seh·ruh·broh·spine·uhl floo·uhd). A group of special cells called choroid plexus are located within the fluid-filled pockets, called ventricles and are responsible for most of the CSF’s production. CSF protects and nourishes the brain.
The brain contains four ventricles—two lateral ventricles located on each side and a third and fourth ventricle located in the midline. The CSF flows in a circuit from one ventricle to another through channels, eventually finding its way to the outside of the brain from the fourth ventricle, where it surrounds and cushions the brain and spinal cord. The CSF eventually returns to the blood through other special cells, called arachnoid granulations, located within the coverings of the brain.
Under normal circumstances, the amount of CSF produced is balanced by the amount returned to the bloodstream, keeping the amount of CSF within the ventricles steady.
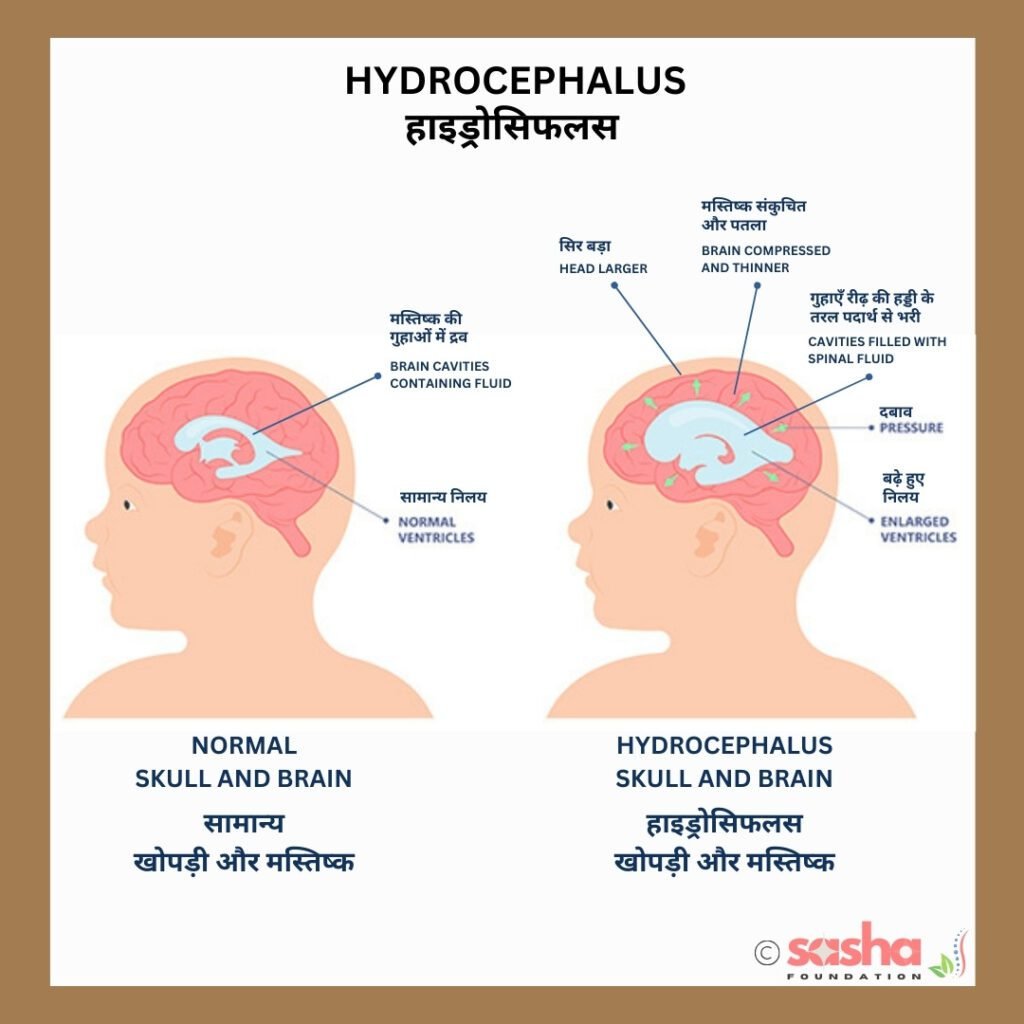
Hydrocephalus occurs when there is an obstruction to the flow of CSF, causing fluid to build up within the cavities of the brain. This fluid build-up can cause pressure on the brain tissues and bones of the skull.
Most children (about 85%) with myelomeningocele will have Hydrocephalus. The accumulation of fluid often doesn’t become significant until after the myelomeningocele has been surgically closed, which means it may not be noticeable until several days or weeks after your child’s birth.
What are the causes of Hydrocephalus?
- Blockage in Ventricles: The blockage of the flow of CSF can occur from one ventricle to another or from ventricles to other spaces in the brain.
- Arachnoid Granulations: The arachnoid granulations are clogged up.
- Absorption Issue: The CSF imbalance can less commonly be due to problems in absorbing CSF. Absorption problems are usually a result of inflammation of brain tissue.
- Overproduction: Even rarer, the overproduction of CSF can cause an imbalance. In these cases, cerebrospinal fluid is produced more quickly than it is absorbed.
What are the signs and symptoms of Hydrocephalus?
The following are the most common symptoms of Hydrocephalus in babies. However, signs and symptoms will vary with age and from individual to individual. Symptoms of hydrocephalus may include:
- A full or bulging fontanelle (soft spot located on the top of the head)
- Seizures
- Enlarged head size
- Bulging eyes and the inability of the body to look upward with the head facing forward
- Headache
- Fever
- Increased irritability
- Vomiting
- Drowsiness
- Loss of previous abilities
- Change in appetite
- Prominent scalp veins
- High-pitched cry
How is Hydrocephalus detected and monitored?
In some cases, the excess CSF is pretty evident and symptomatic and in other cases, excess CSF is evident but in small quantity and asymptomatic. Some kids or adults can handle the increased CSF better than others. Because of this, there is no benchmark for ventricular enlargement and thus treated differently.
As compared to adults, in infants, the plates of the skull are not yet fused. The plates therefore can shift and accommodate the excess cerebrospinal fluid and thus lessen the impact on the brain.
In children, Hydrocephalus is detected and monitored through regular measurement of the child’s head circumference (distance around your child’s head). As fluid accumulates, a child’s head circumference increases in size. Hydrocephalus can also be detected by scanning of the head. The enlarged ventricles can be seen on a Computerized Tomographic (CT) or Magnetic Resonance Imaging (MRI) scan.
How is Hydrocephalus treated?
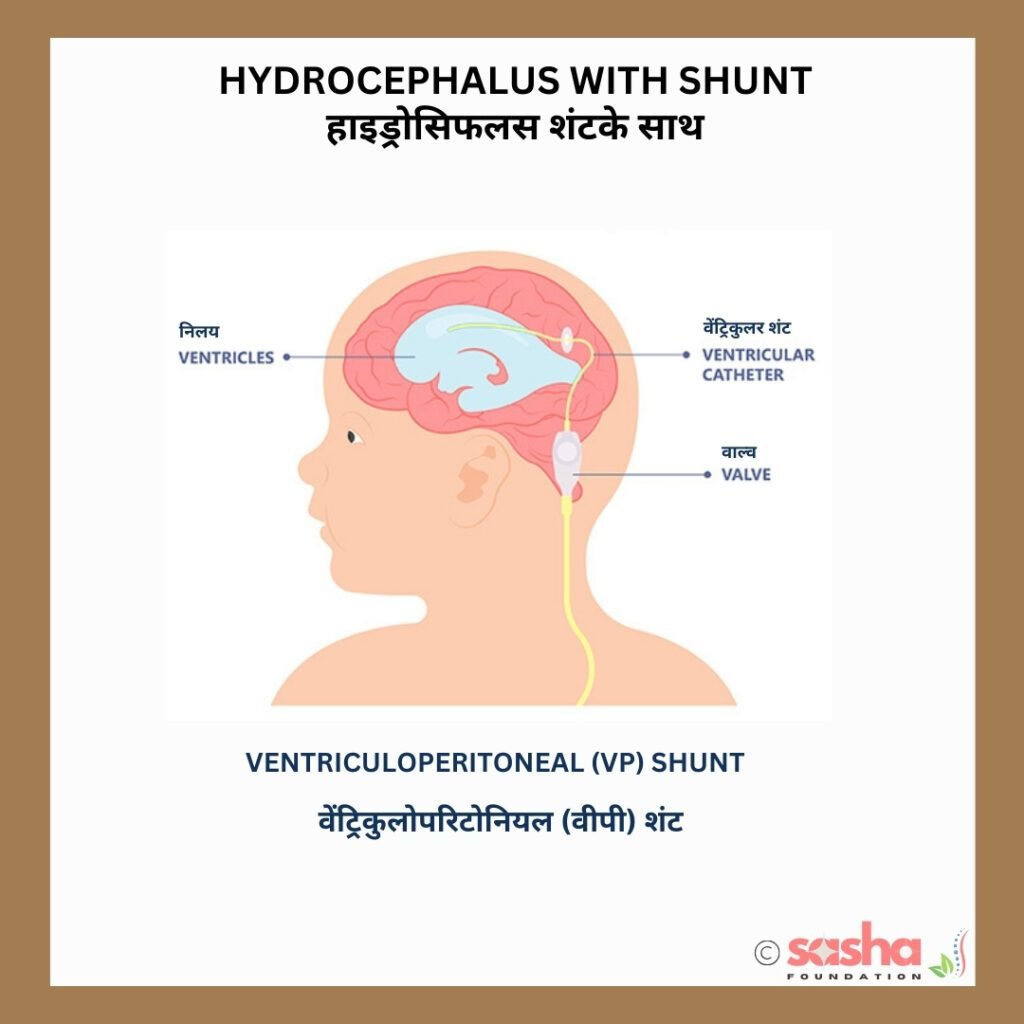
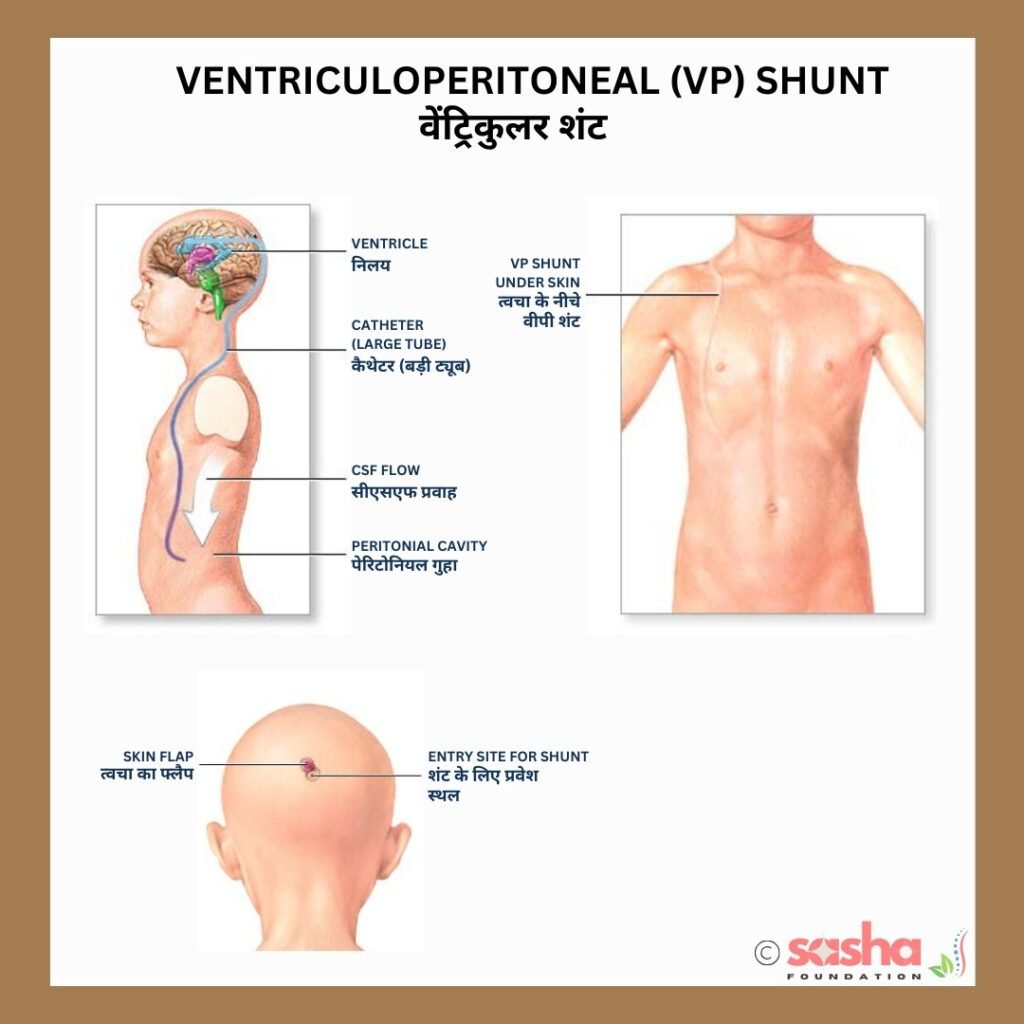
Hydrocephalus is usually treated by inserting a shunt to drain the excess CSF from the brain (ventricles) to another part, of the body, often the abdominal cavity (stomach). Shunts have three parts:
- A short catheter: A short catheter called a ventricular catheter is inserted into a ventricle, most commonly into one of the two lateral ventricles.
- A valve: This one-way valve controls the flow of CSF and is attached to the ventricular catheter mentioned above. There are many types of valves.
- A long tube: This long tube is responsible for transporting the CSF to another location in the body where it can be reabsorbed.
These are internal shunts, they are inserted through small incisions and tunnelled under the skin. The shunts have no external parts on the outside of the body. Draining the excess fluid relieves the symptoms of Hydrocephalus that are present.
Though sometimes this procedure could be done before the closure, commonly takes place following surgical closure of the myelomeningocele.
What are the different types of shunts?
The most common type of shunt is:
- Ventriculoperitoneal (VP) Shunt: The VP shunt transports CSF from the ventricle to the body’s abdominal cavity. Note that the shunt is not inserted into the stomach itself. The CSF within the abdominal cavity is reabsorbed back into the bloodstream.
Other, less common, types of shunts are:
- Ventriculoatrial (VA) Shunt: The VA shunt transports CSF directly into a vein, usually in the neck (jugular vein) or under the collarbone.
- Ventriculopleural Shunt – This shunt transports CSF to the chest cavity that surrounds the lungs, from where it is reabsorbed back into the bloodstream.
There isn’t much data on why one shunt works better than another and so surgeons are therefore free to pick the shunt they think will work best for the person.
What are the different types of shunt valves?
Several types of shunt valves are available and all of these valves have just two purposes:
- Ensure that the CSF moves only in one direction – from the head to another part, of the body.
- Control the amount of CSF allowed to drain.
There are two main types of shunt valves: fixed and adjustable. Fixed valves drain fluid at a set pressure, while adjustable valves allow, the pressure setting to be changed.
Fixed Valves
There are two kinds of fixed valves:
Fixed differential pressure valves: Also known as mono pressure valves, these valves have a ball and spring mechanism that drains fluid when the pressure in the brain is too high.
Fixed differential pressure valves with an antisiphon mechanism: These valves have an antisiphon mechanism to prevent fluid from being pulled back into the brain.
Adjustable/Programmable Valves
- Magnetic externally adjustable valves: These valves have mechanical parts that can be adjusted from outside the body using a magnetic tool.
- Non-magnetic externally adjustable valves: These valves can be adjusted without using an external magnetic field.
- Programmable differential pressure valves: These valves can be adjusted by a doctor using an external adjustment tool.
The type of shunt valve that is best for a patient depends on many factors, including the patient’s condition, age, and size.
How is a Ventricular Shunt inserted?
The ventricular shunt is inserted through the brain and into the ventricle through a small incision and burr hole in the skull. The catheter is most commonly placed through one of three sites on the head:
- The top of the head (in an infant this is near the edge of the soft spot).
- Above and behind the ear.
- The back of the head.
There is not much data on which place works better than another, so the
Studies have not determined whether one place works better than another and so surgeons are therefore free to pick where to place the ventricular catheter.
How long does the shunt stay in the body and will a replacement be needed?
A child who doesn’t need a shunt by the time they are five months old probably will never need one. If a person requires a shunt, it will be lifelong and always be necessary … a shunt is for life. A child may need their shunt replaced a few times as the long tube transporting the CSF can become short as the child grows. Surgery may be necessary to remove or replace the shunt or lengthen it as needed.
Shunts generally work well but problems can arise. Shunts can become infected, blocked or, they can twist and break. Swelling or redness along the shunt tract in people who already have a shunt, tells that there is an imbalance of CSF and immediate attention is needed.
About 40% of shunts fail in the first year for a variety of reasons. If this happens, CSF will begin to accumulate again. Problems may occur suddenly or develop gradually.
Both in, adults and children, the symptoms mentioned earlier are tell-tell signs of a problematic Hydrocephalus.
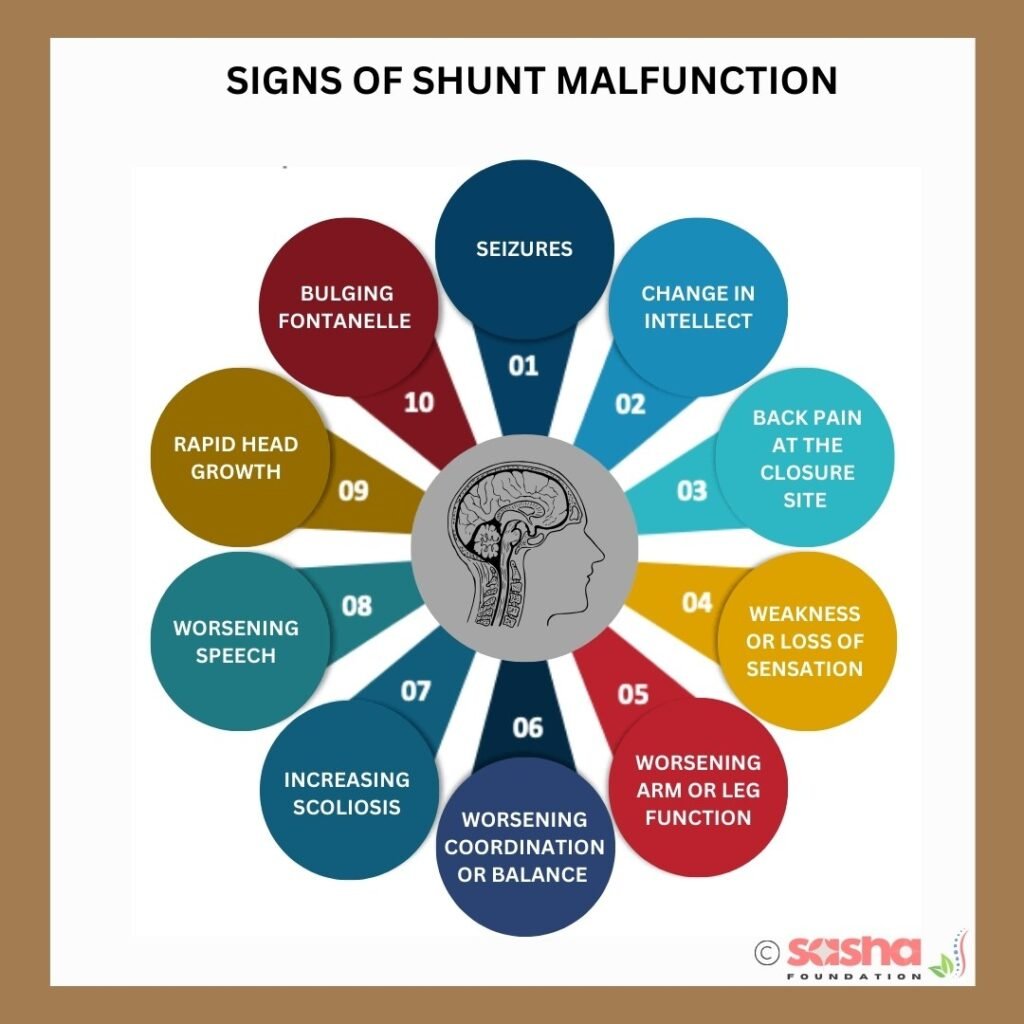
What are the signs of shunt malfunction?
Signs of shunt malfunction most commonly include a headache, nausea and/or vomiting. Less common signs of a shunt problem in somebody with Spina Bifida may include:
- Seizures
- A significant change in intellect, school performance or personality
- Back pain at the Spina Bifida closure site
- Weakness or loss of sensation
- Worsening arm or leg function
- Worsening coordination or balance
- Increasing scoliosis
- Worsening speech or swallowing difficulties.
Infants may in addition have
- Rapid head growth
- A full or bulging fontanelle (soft spot located on the top of the head)
- Unusual irritability
- Repeated vomiting
- Bulging eyes and the inability of the body to look upward with the head facing forward
- Periods in which the baby stops breathing (called apnea)
- Difficulty swallowing
- A hoarse or weak cry

However, a small percentage of people with Spinal Bifida may have a shunt malfunction without any noticeable changes in ventricular size on CT or MRI scans. Therefore, families and healthcare providers must remain vigilant and closely monitor the person’s symptoms, particularly if they resemble those experienced during prior shunt issues.
Since the symptoms of shunt malfunction, can resemble those of Chiari malformation, it is crucial to consider shunt malfunction as a potential cause of any unexplained deterioration in brain or spinal cord function.
A head ultrasound (only available in infants when the fontanelle is still open), CT or MRI scan will show the CSF build-up as an increase in the size of the ventricles. If available, a baseline scan performed when the shunt was working well (if available) should be compared with the present scan, looking for changes in ventricular size.
Some people with shunted Hydrocephalus can develop a slit or stiff ventricle syndrome. In slit ventricle syndrome excess CSF drainage leads to very small or slit ventricles. The ventricles may have become less compliant over time due to repeated cycles of expansion and contraction causing temporary ventricular shunt blockages or malfunction repeatedly.
What are the chances and signs of shunt infection?
Shunt infection is a significant complication, affecting 5% to 10% of shunt operations. The incidence of these infections is higher in infants compared to older children and adults. Notably, 70% of shunt infections occur within the first two months post-operation, and 80% within the first six months. The most common cause of shunt infections is the skin bacterium Staphylococcus epidermidis.
Many people with shunt infections show signs of a shunt malfunction. Additional signs of an infection are:
- Fever
- Neck stiffness
- Pain, tenderness, or redness along the shunt tract
- Drainage from the shunt incisions or tract
- Abdominal pain.
How is shunt infection tested and treated?
CSF will be collected from the shunt and will be sent for CSF culture. The culture report usually takes 3 – 7 days. An increase in the white blood cell count suggests an infection. Infections are treated with antibiotics plus removal and replacement of the entire shunt system. There are two ways of doing this:
Method 1: Antibiotics treatment is started and the entire shunt system is removed and replaced with a temporary external ventricular drainage catheter (EVD) that drains to an external bag. After the antibiotic course is over this EVD is removed and replaced with a new shunt. This process requires two surgeries.
Method 2: In this method, they keep the working shunt in place until the end of the antibiotic treatment. After the antibiotic course, they remove and replace the old shunt. This process requires only one surgery but is slightly less successful when compared to the first method.
What should you do if your child has Hydrocephalus?
As the symptoms or signs of shunt malfunction can look similar to those of a Chiari malformation, it is important to consider a shunt malfunction as a potential cause of any deterioration in brain or spinal cord function without another clear cause.
Parent’s (and particularly mom’s) perspective about shunt problems is very important — particularly if the symptoms are similar to those that occurred with prior shunt problems.
- As a parent, you should keep a scan that was performed when the shunt was working well so that it acts as a baseline and helps in comparing the current and future scans, looking for changes in ventricular size.
- As a parent, be aware that shunt problems can cause many symptoms that may not, at first glance, appear to be shunt-related.
- Be on the lookout for shunt problems, and make sure the shunt is working before performing other neurosurgical treatments, such as those for Chiari or spinal cord tethering.
Please Note
The information provided on our website is not intended as medical advice for any individual. Since specific cases may differ from the general information presented, SASHA recommends consulting a qualified medical or other professional for personalized advice.
About the Author
Raul/DJ Vivek
Meet Vivek Bharadwaj, a remarkable individual who has defied the odds and soared to new heights despite living with Spina Bifida. As the founder of the Sasha Foundation, Vivek tirelessly advocates for others facing similar challenges. His unwavering commitment to support, awareness, and empowerment had made a lasting impact on the Spina Bifida community.
FAQ
What is Hydrocephalus?
Hydrocephalus is a condition where cerebrospinal fluid (CSF) builds up in the brain’s ventricles, which can cause brain damage or death.
Is there an effective cure for Hydrocephalus?
No, there is no cure for hydrocephalus, but it can be treated with surgery
Does Hydrocephalus qualify for disability?
Yes, hydrocephalus can qualify as a disability, and you may be eligible for disability benefits.
Why do people get Hydrocephalus?
Hydrocephalus, also known as “water on the brain”, occurs when cerebrospinal fluid (CSF) builds up in or around the brain.
Is Hydrocephalus deadly? Can you live a normal life with it?
Hydrocephalus if treated on time, is not deadly and yes you can live a normal life though you have to be vigilant towards blockage and infections.
Can a baby with Hydrocephalus lead a normal life?
Yes, many children with hydrocephalus can lead normal lives with the right care and treatment.
Is Hydrocephalus hereditary?
Yes, hydrocephalus can be hereditary. In fact, genetic factors are thought to play a major role in the development of hydrocephalus.
Why is Hydrocephalus more serious in adults?
Hydrocephalus is considered more serious in adults because the skull is fully fused and cannot expand to accommodate excess cerebrospinal fluid (CSF), leading to increased intracranial pressure that can significantly damage brain tissue
Does Hydrocephalus cause any psychiatric disorders after shunting?
Is mental illness commonly associated with Hydrocephalus?
No, there is no data to suggest this.
Can someone with Hydrocephalus shunt join the police or armed forces?
Joining the police or armed forces for someone with shunted Hydrocephalus is going to be impossible because both, police and armed forces disqualify individuals with certain medical conditions that may impair their ability to serve effectively.
What is someone with hydrocephalus’s life expectancy?
Most newborns born with hydrocephalus will have a normal lifespan, and approximately 40 to 50% will have normal intelligence.
Does Hydrocephalus affect memory?
No, it does not.






Leave a Reply
You must be logged in to post a comment.