In this article, we will answer the most common question we get, “Will my child walk?”
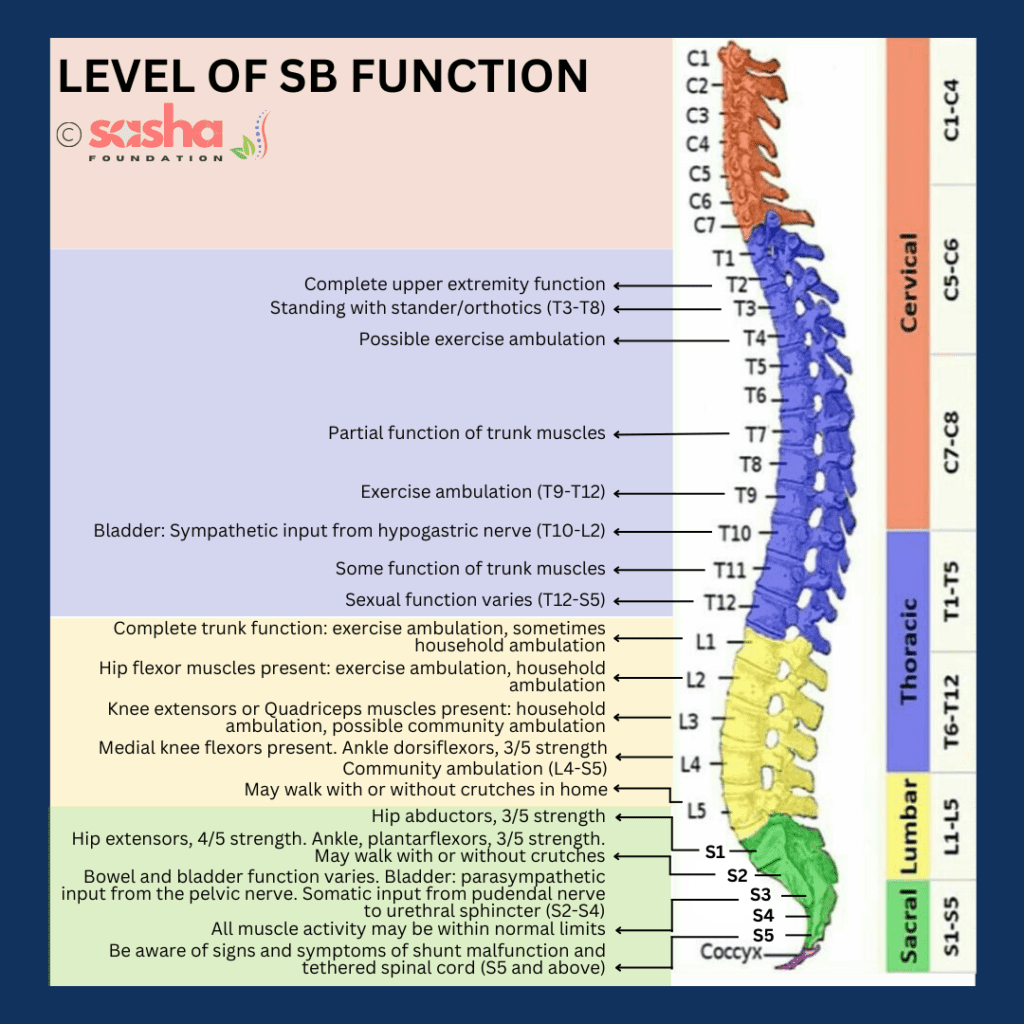
MRI level/ functional level
Myelomeningocele affects the development of a child’s brain and spine differently than other children. When you first consult with doctors and nurses, they might mention your child’s MRI lesion level. This term refers to the lesion’s (Spina Bifida’s) location on your child’s spine as seen on scans. We use this information during antenatal consultations to predict your child’s condition at birth.
After your baby is born, healthcare providers will observe and assess their movements to understand how myelomeningocele affects them. By identifying which muscles are functioning, healthcare providers can determine your baby’s “functional level.” This description of muscle activity is more useful for predicting long-term outcomes than the MRI lesion level. Functional-level assessments become more accurate from around six months of age.
A common question parents ask the Sasha Team is, “Will my child walk?” While assessing the functional level provides insight, walking is influenced by multiple factors beyond just the functional level. These factors include the presence of hydrocephalus and the alignment of your child’s bones and muscles (postural alignment). While this data is as accurate as possible at this stage of development, each child is unique and may exhibit differences from their MRI level.
If your child’s muscle nerves are non-functional, they cannot be repaired and will have permanent weakness.
It’s important to recognize that children with Spina Bifida (myelomeningocele) who are able to walk may need additional supports like leg splints, such as ankle and foot orthoses (AFOs).
How the functional level of the lesion may affect your child?
Your child’s functional level of the lesion will be continuously assessed and monitored by their physiotherapist, orthopaedic surgeon, and paediatrician. It’s important to note that the functional level may deteriorate over time. The spine consists of 33 vertebrae, which are divided into different regions known as cervical, thoracic, lumbar, and sacral.
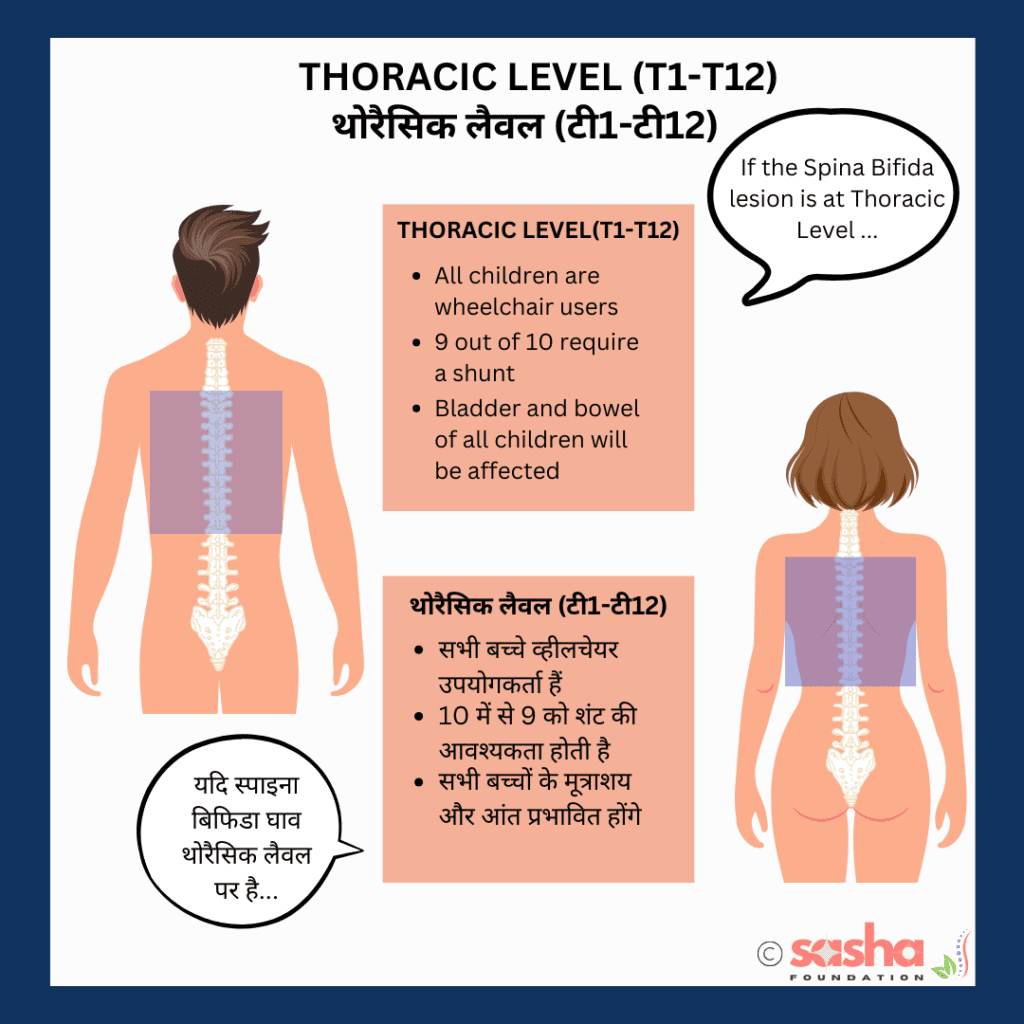
If your child’s functional level is located at the Thoracic level (T1 – T12) your child may:
- Be unable to stand up without support.
- Need a wheelchair to move around.
- Have orthopaedic needs like spinal curves e.g. scoliosis, hip dislocations, knee contractures, and talipes (club feet).
- Require help to do activities such as dressing and bathing.
- Require help in school to do everyday activities, e.g. toileting.
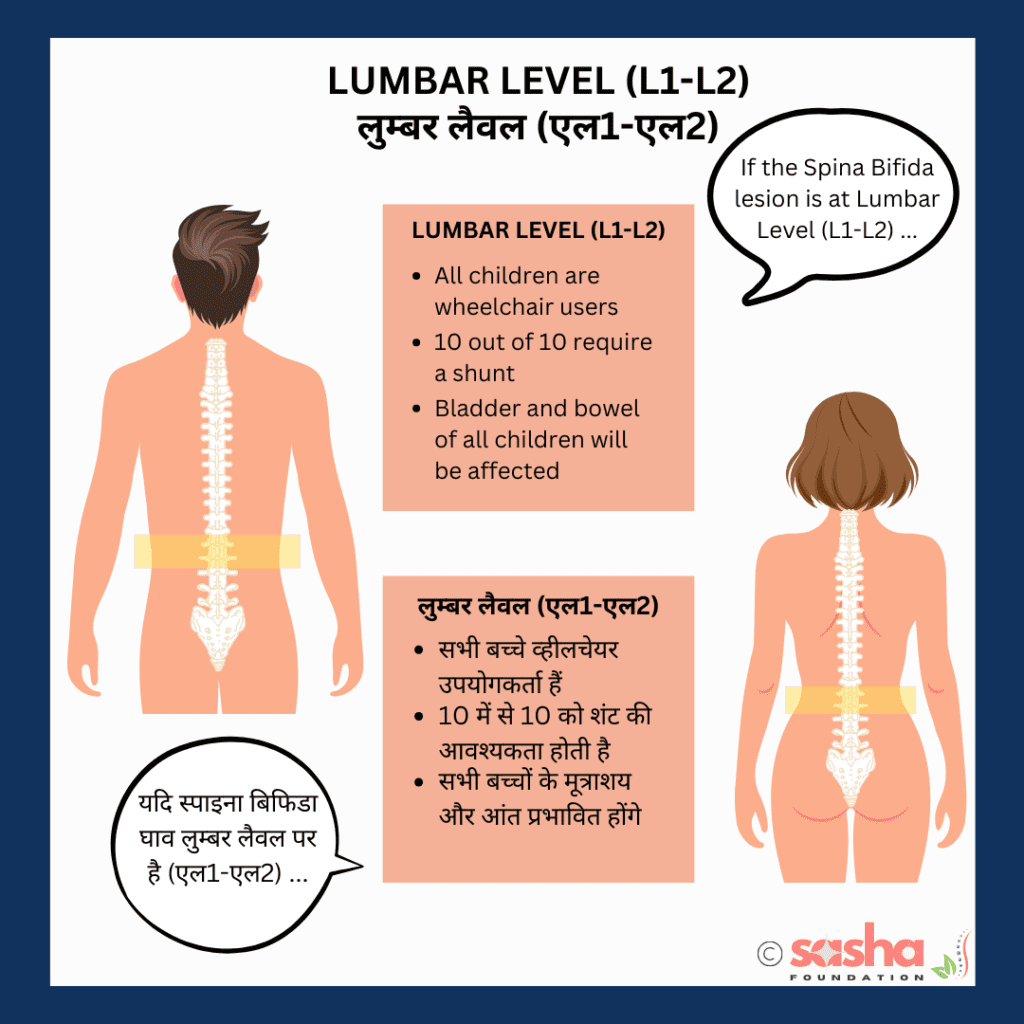
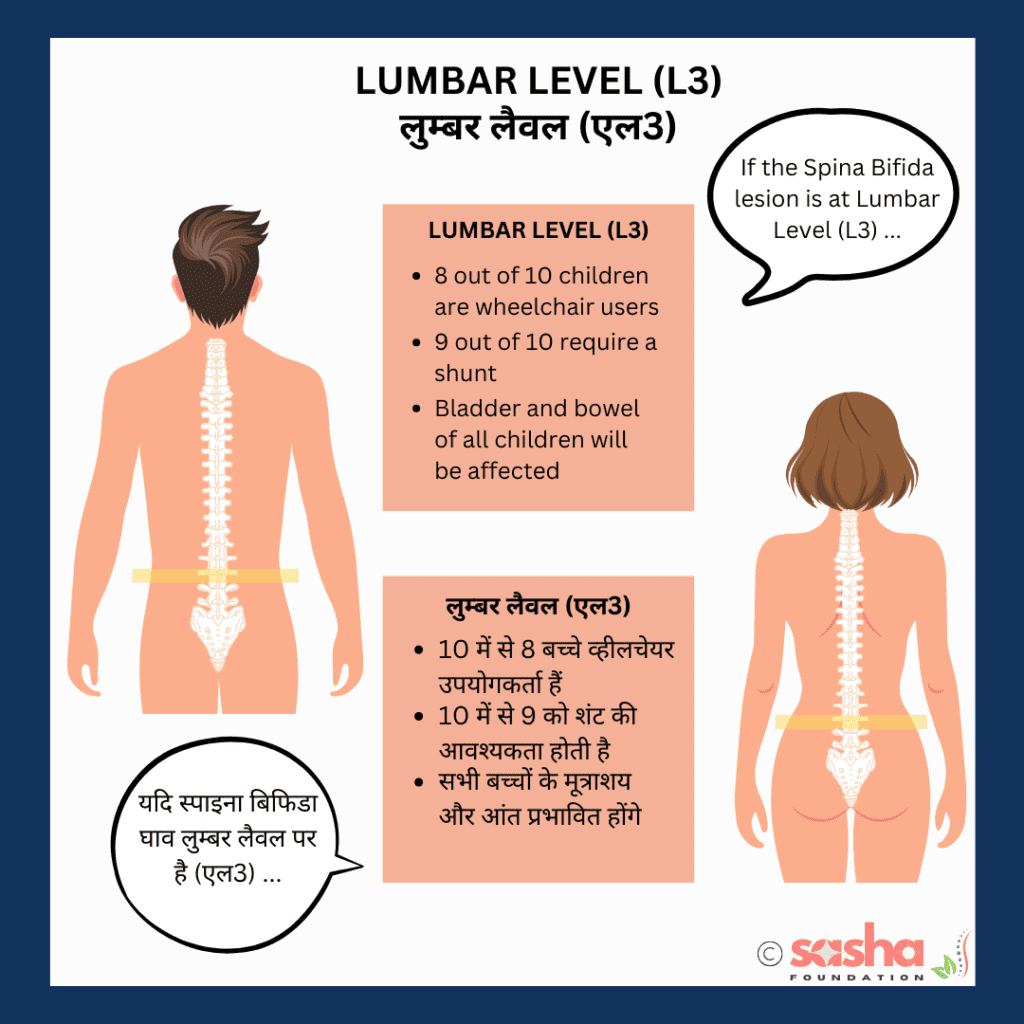
If your child’s functional level is located at Lumbar levels (L1, L2, L3) your child
may:
- Will require supports to stand up e.g. frame, crutches, orthoses (foot, knee and or hip supports)
- Need a wheelchair to move around
- Have orthopaedic needs which may include spinal curves e.g. scoliosis, hip dislocations, knee contractures, talipes (club feet)
- Will require help to do activities such as dressing and bathing.
- Will require help in school to do everyday activities e.g. toileting.
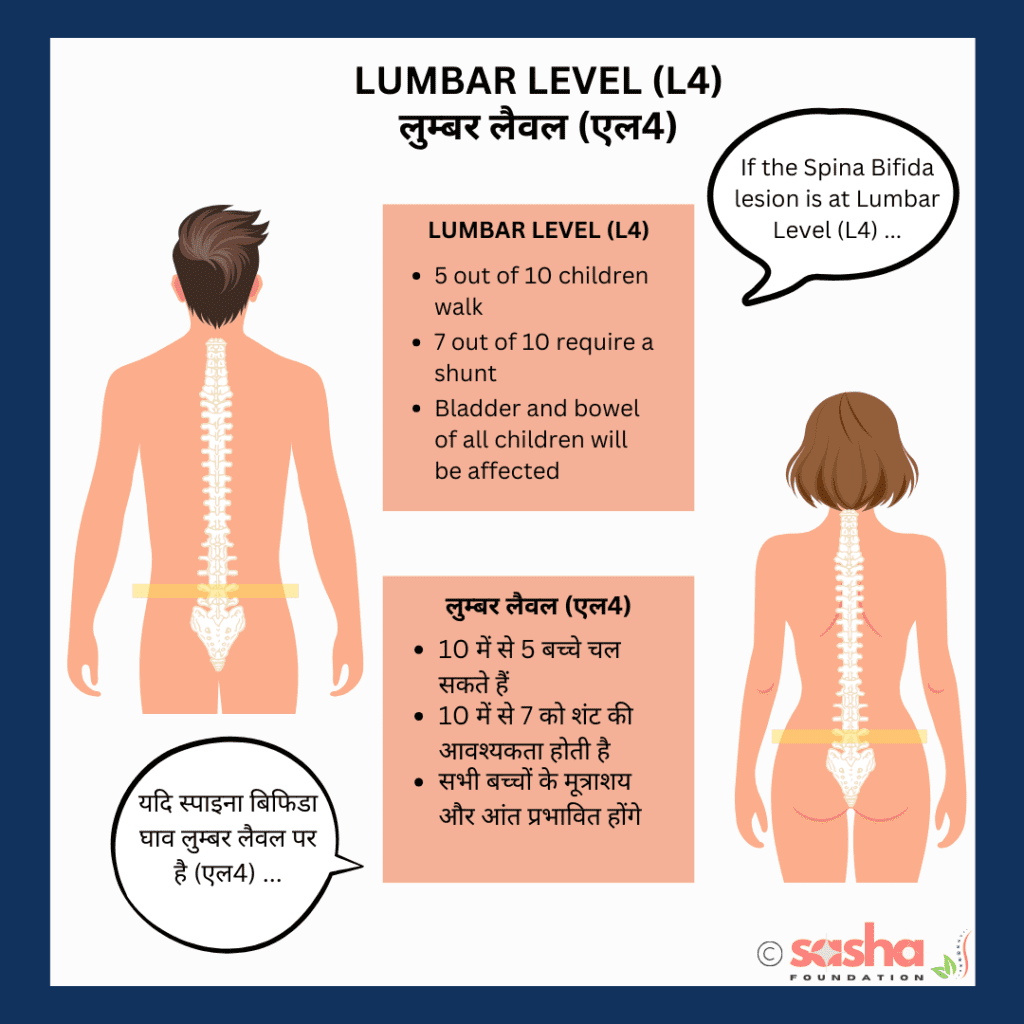
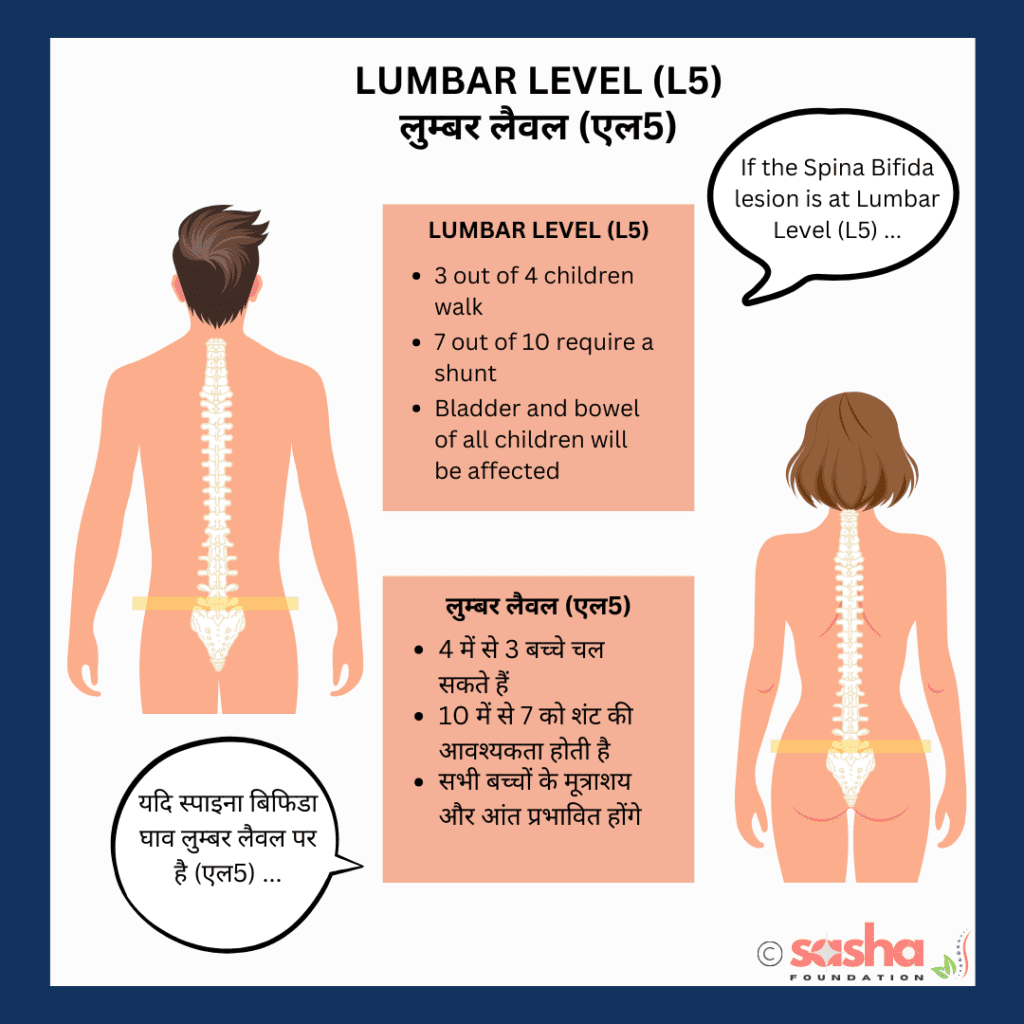
If your child’s functional level is located at Lumbar levels (L4, L5) your child may:
- Will require supports to walk including orthoses e.g. ankle and knee supports.
- Need a wheelchair for long distances due to fatigue.
- Have orthopaedic needs like hip dislocations, knee contractures, and talipes (club feet).
- Will require some assistance to do activities such as dressing and bathing.
- Will require help in school to do everyday activities e.g. toileting.
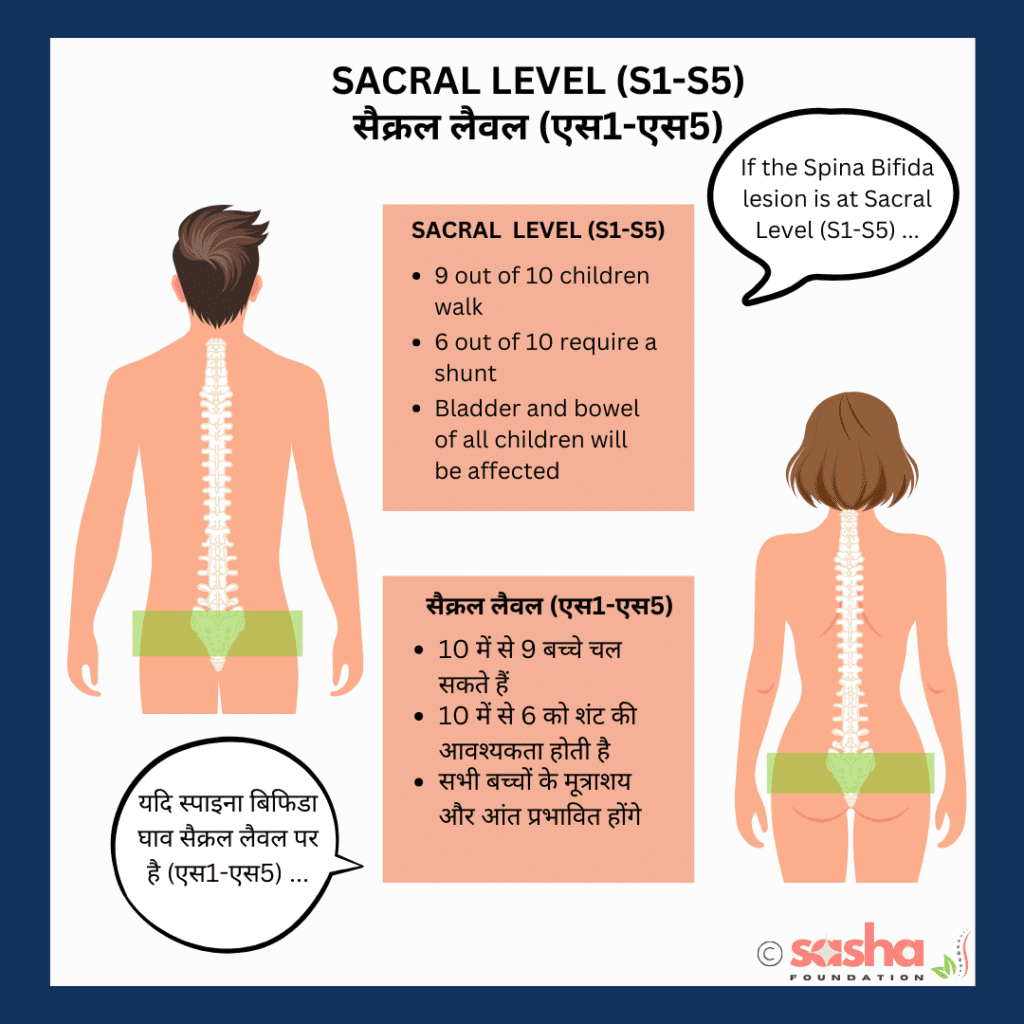
If your child’s functional level is located at Sacral levels (S1, S2) your child may:
- Stand without supports.
- Walk without supports.
- Have orthopaedic needs which may include toes and feet problems.
Source – The data above is based on 10 years of information gathered in Temple Street Children’s University Hospital.
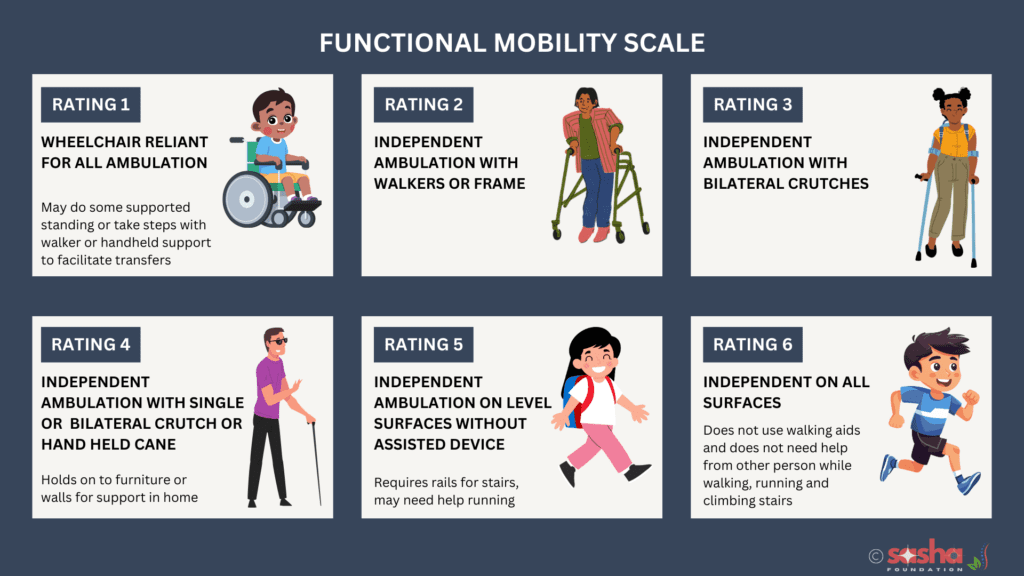
Gaining Insight into Functional Mobility through the Perspective of Lesion Levels
The information below is provided to help you, as a parent, to have informed and productive conversations with your healthcare providers.
- If your child’s functional level or the Spina Bifida lesion is located at the thoracic level (T1 – T12) your child will be at Rating 1 on the functional mobility scale.
- If your child’s functional level or the Spina Bifida lesion is located at the lumbar level (L1, L2) your child will be at Rating 1 to Rating 2 on the functional mobility scale. Will need a wheelchair when outside and might be able to move around at home with walkers or crutches.
- If your child’s functional level or the Spina Bifida lesion is located at the lumbar level (L3) your child will be at Rating 1 to Rating 3 on the functional mobility scale. Will need a wheelchair when outside and might be able to move around at home with walkers or crutches.
- If your child’s functional level or the Spina Bifida lesion is located at the lumbar level (L4, L5) your child will be at Rating 1 to Rating 5 on the functional mobility scale. Some will need a wheelchair when outside, some will be able to move around with walkers or crutches and some will walk independently without any help. We have seen some cases of L5 where the person can run also (with some difficulty).
- If your child’s functional level or the Spina Bifida lesion is located at the sacral level (S1 – S5) your child will be at Rating 1 to Rating 6 on the functional mobility scale. Some will need a wheelchair when outside, most will be able to move around with walkers or crutches and some will walk independently without any help. Seeing children at Rating 1 here is not that often.
Please Note
The information provided on our website is not intended as medical advice for any individual. Since specific cases may differ from the general information presented, SASHA recommends consulting a qualified medical or other professional for personalized advice.
About the Author
Raul/DJ Vivek
Meet Vivek Bharadwaj, a remarkable individual who has defied the odds and soared to new heights despite living with Spina Bifida. As the founder of the Sasha Foundation, Vivek tirelessly advocates for others facing similar challenges. His unwavering commitment to support, awareness, and empowerment had made a lasting impact on the Spina Bifida community.
FAQ
What is Myelomeningocele?
Myelomeningocele is a severe form of Spina Bifida where the spinal cord and meninges protrude through an opening in the spine. This condition is usually diagnosed prenatally or at birth and requires immediate medical attention.
What causes Myelomeningocele?
The exact cause is unknown, but it is believed to result from a combination of genetic, nutritional (such as folic acid deficiency), and environmental factors.
What are the symptoms of Myelomeningocele?
Symptoms can vary but often include muscle weakness or paralysis in the lower limbs, bladder and bowel dysfunction, hydrocephalus (accumulation of cerebrospinal fluid in the brain), and orthopaedic complications like scoliosis and clubfoot.
Is there a cure for Myelomeningocele?
No, there is not. There are measures that one can take.
How is Myelomeningocele diagnosed?
It is typically diagnosed through prenatal screening tests such as ultrasound and blood tests, or immediately after birth through physical examination and imaging tests.
What treatments are available for Myelomeningocele?
Treatment options may include surgery to close the opening in the spine, management of hydrocephalus, physical therapy, and addressing orthopaedic issues.
Can children with Myelomeningocele walk?
Some children with Myelomeningocele may walk with or without support, depending on the severity and location of the lesion. Others may require mobility aids such as wheelchairs.
How can Myelomeningocele be prevented?
Taking folic acid supplements before and during early pregnancy can significantly reduce the risk of neural tube defects, including Myelomeningocele.
What is the long-term outlook for children with Myelomeningocele?
The long-term outlook varies depending on the severity of the condition and the effectiveness of treatments. Early intervention and ongoing medical care can help improve the quality of life.






Leave a Reply
You must be logged in to post a comment.