This article will discuss Spinal cord tethering and Tethered Cord Syndrome (TCS). I will also answer a common question we get, “Should I get my child operated?”
Spinal Cord Tethering
Spinal Cord Tethering occurs when the spinal cord becomes attached to the spinal column through surrounding structures. Normally, the spinal cord hangs loosely in the canal, allowing it to move freely with growth, bending, and stretching. However, this movement is restricted in a tethered cord, as the cord is pulled tightly at one end. This reduces blood flow to the spinal nerves and causes damage to the spinal cord due to both stretching and diminished blood supply.
Spinal Cord Tethering can occur both before and after birth, affecting children and adults alike. Spina Bifida Occulta children have the least possibility of Spinal Cord Tethering.It most commonly happens in the lower (lumbar) region of the spine. For children, a tethered cord stretches as they grow, while for adults, it stretches during everyday activities such as bending and stretching.
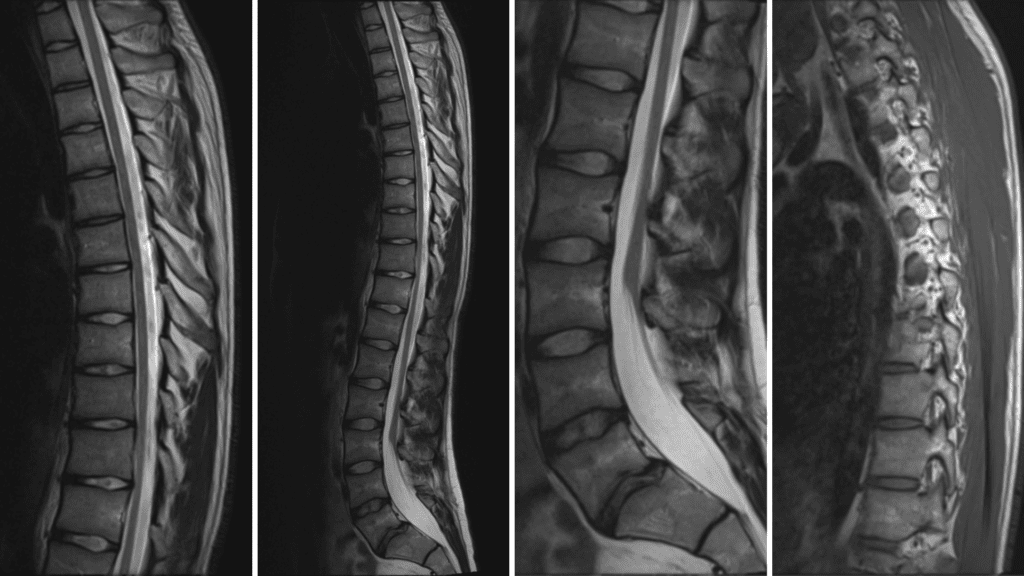
Case courtesy of Bruno Di Muzio
What is Tethered Cord Syndrome?
Tethered Cord Syndrome is a neurological disorder resulting from spinal cord malformations. This condition restricts the spinal cord’s movement within the spinal canal, causing it to stretch as the spine grows. This tension, or stretching, of the spinal cord, due to the increased length of the spine can lead to nerve damage, pain, sensory disturbances, significant muscle weakness, and incontinence known as Tethered Cord Syndrome (TCS).
Myelomeningocele and Tethered Cord Syndrome
By definition, all children with Myelomeningocele have a tethered cord, as this is an inherent aspect of their anatomy. However, this does not mean that these individuals will have symptoms or problems related to the Tethered Cord Syndrome (TCS), and thus often do not require any treatment.
This happens because, in children with Myelomeningocele, the spinal cord terminates lower than it does in the general population. The spinal cord at birth is low-lying, or tethered. Additionally, these children often have scarring at the end of the spinal cord due to the surgical procedure required to close the neural tube (Spina Bifida Surgery).
Tethered Cord Syndrome (TCS) is rarely an issue for children with Myelomeningocele and is usually asymptomatic. However, in rare instances, these children may develop symptoms as they grow. The tension, or stretching, of the spinal cord, due to the increased length of the spine can lead to progressive neurological, urological, or orthopaedic deterioration. If a symptomatic tethered cord (tethered cord syndrome) is left untreated, it can lead to progressive, permanent spinal cord damage.
What causes tethering in other forms of Spina Bifida?
Tethered Cord Syndrome (TCS) in milder forms of Spina Bifida can occur due to the gradual strain placed on the spinal cord over time. It may also result from the narrowing of the spinal column (stenosis) or the presence of bony spurs.
What are the symptoms of Tethered Cord Syndrome?
Symptoms of a tethered cord syndrome may include:
- Loss of muscle mass (muscle atrophy) or weakness.
- Loss of muscle function.
- Difficulty walking.
- Increased muscle tone/stiffness. You may notice that some of your child’s leg muscles feel tighter.
- Severe radiating and shooting leg or back pain.
- Loss of sensation or numbness. You may notice that your child cannot detect touch or hot and cold sensations in parts of their lower limbs.
- Rapid progression of curvature of the spine (scoliosis)
- Changes in bowel or bladder function causing changes in their toileting abilities
- Progressive Changes in the way, the feet look, like higher arches or curled toes. Change in the way shoes fit.
How is Tethered Cord Syndrome diagnosed?
Tethered Cord Syndrome (TCS) is initially diagnosed through clinical evaluation, followed by, a series of scans and tests to confirm the diagnosis.
Step One – Manual Muscle Testing (MMT)
Manual Muscle Testing (MMT) is a diagnostic tool that assesses muscle strength and can help determine a variety of things, including:
- Muscle weakness
- Muscle function
- Muscle response to intervention
- Immediate neurological responses
Manual muscle testing (MMT) of children born with Spina Bifida is usually regularly done. Manual Muscle Testing (MMT) is done to establish a baseline, which can aid in detecting changes that might indicate Tethered Cord Syndrome (TCS) in future assessments. MMT is performed by a doctor who applies resistance to a muscle group while the patient contracts it. The doctor scores the muscle’s strength, on a scale from 0 to 5.
Step Two – CT or MRI Scans
For a person with myelomeningocele and shunted hydrocephalus:
If a child with myelomeningocele and shunted hydrocephalus shows clinical deterioration, the initial step is to assess the shunt’s functionality. Shunt malfunction can manifest symptoms similar to those of a tethered cord. So, check the shunt first! So, the first test is usually a Computed Tomography (CT) or Magnetic Resonance Imaging (MRI) scan, of the brain. Once the shunt malfunction is ruled out, an MRI, of the spine, is performed.
For a person with myelomeningocele:
An MRI, of the spine, is performed.
The MRI is done to show the neurosurgeon the anatomy of the tethering and to exclude other abnormalities such as a syringomyelia (syrinx), split cord malformation, or a dermoid cyst (small tag of skin in the area around or within the spinal cord).
Step Three – Additional Studies
X-rays:
The doctor may recommend an X-ray of the spine to identify any other bony abnormalities or to monitor the progression of scoliosis.
Urodynamic Studies:
A Urodynamic study could be performed, to compare and document changes with previous studies. This will help provide a pre-surgical baseline.
When is Tethered Cord Syndrome surgery performed? And who does it?
Tethered Cord Syndrome (TCS) is treated surgically by an experienced neurosurgeon. The decision to untether requires some clinical judgment. After reviewing the diagnostic studies, the neurosurgeon may decide to untether the spinal cord. During the surgery, the neurosurgeon makes an incision in the lower back and removes scar tissue to detach (release the tension) the spinal cord from the spinal canal.
What are the complications of Tethered Cord Syndrome surgery?
Untethering surgery is generally considered safe. However, scarring can complicate dissection, and the abnormal anatomy can be challenging for most experienced surgeons. The more common complications include infection and bleeding. However, serious complications can involve damage to the spine and myelomeningocele, which may lead to worsening bladder or bowel function. In some cases, the functional mobility of the lower limbs may also be affected. Additionally, individuals with a shunt may experience shunt malfunction.
Will my child or I need more than one surgery for a tethered spinal cord?
Most people need only one surgery to treat a tethered spinal cord. However, up to 1 in 5 children need more than one surgery. Tethered Cord Syndrome symptoms usually increase or flare up during periods of growth. The pre-adolescent period (ages 7-12) is often the most problematic for Tethered Cord Syndrome.
While all children grow, it is unclear why some develop symptoms and signs of tethering while others do not. It is possible that some children’s spinal cords can tolerate a greater degree of stretching than others. In adulthood, clinical deterioration due to tethering becomes much less frequent, although it can still occur. Re-tethering in adults may result from scar tissue formation, spinal deterioration or injury.
My opinion – Is the surgery safe?
In short, no. This surgery is a double-edged sword that tends to result in negative outcomes. I have witnessed numerous cases, including my own, where the situation has deteriorated from either, good or bad, to worse. I’ve known individuals who, following Tethered Cord Syndrome surgery, have experienced further or complete loss of bladder and bowel control. Additionally, many have endured other complications such as chronic neuropathic pain and loss of lower limb strength, with some transitioning from being able to walk to becoming wheelchair-bound. I’d also like to state that there are cases where this surgery had neither positive nor negative outcomes, and the status quo was maintained.
Please understand that I am not implying that there are incompetent neurosurgeons or that these surgeries were carried out by less skilled professionals. This discussion is not about the surgeons but about you or your child. A surgeon’s primary responsibility is to perform surgeries. When a case is presented, they are inclined to proceed with the operation, as this is their area of expertise and training. It is you, who has to make the informed call as it is you, who will be affected. Sometimes the best move is not to play.
Almost every child with Spina Bifida (Myelomeningocele) shows evidence of tethering on an MRI. Surgical untethering should be considered only if there are extremely loud clinical signs of deterioration, such as unbearable pain, rapid loss of muscle function, severe bending of feet, or rapid loss of bladder or bowel function. This deterioration should be compared with previous MMTs and other studies, like urodynamic studies to make an informed call.
I know numerous neurosurgeons and when spoken to privately, they often express that Tethered Cord Syndrome surgery provides little to no benefit for a Spina Bifida person. Given the associated risks, they generally advise against it in most cases, preferring to leave it untreated. Especially, in Spina Bifida (myelomeningocele) cases often the nerves are all clogged up and there is previous scarring so it is very challenging for a neurosurgeon to release the tension.
The recovery of lost muscle and bladder function is variable and depends on both the degree and length of the neurologic losses before the surgery. Untethering is designed primarily to prevent further deterioration, not to improve spinal cord damage that has already occurred. Yes, the longer deterioration continues, the less likely it is that function will return. Modern microsurgical equipment and techniques have made untethering a fairly routine procedure.
What should you do?
It is essential to establish a data baseline for people with Spina Bifida, to accurately, compare and detect any deterioration. Once a year, you should get Manual Muscle Testing (MMT) and Urodynamic Studies done, especially, if you have a growing Spina Bifida child. Please, don’t waste money on repeating MRIs every year as this will always show a tethered cord syndrome.
We will soon publish an article detailing the initial tests and studies required and those that should be repeated, at regular intervals. Subscribe to our newsletter and get notified when we post new information.
Please Note
The information provided on our website is not intended as medical advice for any individual. Since specific cases may differ from the general information presented, SASHA recommends consulting a qualified medical or other professional for personalized advice.
About the Author
Raul/DJ Vivek
Meet Vivek Bharadwaj, a remarkable individual who has defied the odds and soared to new heights despite living with Spina Bifida. As the founder of the Sasha Foundation, Vivek tirelessly advocates for others facing similar challenges. His unwavering commitment to support, awareness, and empowerment had made a lasting impact on the Spina Bifida community.
FAQ
How can I prevent a tethered spinal cord?
Tethered spinal cords aren’t preventable. They can only be treated.
Can people with Tethered Cord Syndrome live a normal life?
Yes, most people with Tethered Cord Syndrome typically live a normal life and have a typical lifespan.
Should I choose a government hospital or a private hospital for my surgery?
This is a personal choice and depends on factors like your financial background. Many government hospitals, like AIIMS, JJ, PGI etc. have highly skilled doctors and operation theatres with the latest technology. In our opinion, government hospital doctors have a lot more exposure to cases and perform well. We trust government hospitals, as much as we trust private hospitals.
Who should I see for Manual Muscle Testing (MMT), in India?
You should go to a neurologist; a physical therapist can also do this testing.
Who should I see for Urodynamic Studies?
You should go to a urologist.
Is a tethered spinal cord present in everyone with Myelomeningocele?
Yes, because that is in their anatomy.
How many days will I have to stay in the hospital if I opt for Tethered Cord Syndrome surgery?
You might have to stay for 3 – 5 days.
What should I do if there are complications post-surgery?
You should contact your neurologist asap, and follow his instructions.
What is neuropathic pain?
Neuropathic pain, also known as nerve pain or neuralgia, is a type of pain caused by damage to or malfunction of the nervous system. Neuropathic pain could be acute or chronic.
What does it feel like to have neuropathic pain?
Neuropathic pain can feel like a burning or tingling sensation, or a sharp, shooting pain. It is, radiating or throbbing pain, in the lower back, buttocks, legs and feet.
I already have neuropathic pain, what should I do?
You should consult a pain management specialist. The pain management department comes under anaesthesia. Chronic neuropathic pain can be dealt with by oral painkillers and epidural pain block (if it works for you). Get in touch, we will guide you.
Is there a cure for chronic neuropathic pain?
No, there is no cure. Depending on how bad your pain is, chronic neuropathic pain can be dealt with (in most cases) by painkillers, tricyclic antidepressants and epidural pain block (if it works for you). Get in touch, we will guide you.
I need assistance, how do I contact you and is it free?
Please call us. Sasha’s helpline number is mentioned on the website. Our help is free, we don’t charge for guidance or consultation.






Leave a Reply
You must be logged in to post a comment.